Understanding Disorders of Platelets
This video discusses disorders of platelets, including production kinetics, thrombocytopenia, qualitative disorders, immune thrombocytopenia, and diagnosis.
00:00:00 This video discusses disorders of platelets, including platelet production kinetics, thrombocytopenia, and qualitative disorders. It covers the causes of thrombocytopenia and the evaluation of bleeding. The video also mentions specific conditions such as neonatal thrombocytopenia and genetic/congenital thrombocytopenia.
💡 Platelet kinetics: average lifespan is 7 to 9 days, removed by circulation from the monocyte macrophage system.
💡 Thrombocytopenia: can result from disorders of platelet production and lifespan (quantitative disorders) or feck morphology and function (qualitative disorders).
💡 Evaluation of thrombocytopenia: bleeding is immediate following injury, petechiae are specific to platelets.
💡 Causes of thrombocytopenia in newborns: impaired production, consumption and sequestration, immune destruction, genetic and congenital factors.
00:05:59 The video discusses the disorders of platelets, specifically immune thrombocytopenia in infants and children. It covers the diagnosis, management, and risk factors. Maternal ITP and neonatal alloimmune thrombocytopenia are also mentioned.
🔑 Immune thrombocytopenia usually occurs in otherwise healthy infants or children, with no other abnormalities observed during physical examination.
🔑 Neonatal immune thrombocytopenia is diagnosed in neonates with a platelet count less than 50,000, who are otherwise healthy with no other findings.
🔑 The management of immune thrombocytopenia involves maintaining platelet counts above thirty thousand, with transfusion of maternal platelets being the gold standard.
00:11:57 Disorders of Platelets: Autoreactive T cells cause B cells to generate antibodies which attach to platelets, leading to their clearance. Children with ITP usually recover within a few weeks.
Disorders of platelets involve autoreactive T cells, B cells generating antibodies, and glycoproteins on the platelets' surface.
Symptoms of ITP include acute thrombocytopenia, reduced platelet count, and mucosal bleeding.
Treatment options for ITP include observation, corticosteroids, IVIG, anti D immunoglobulin, splenectomy, rituximab, and thrombopoietin receptor agonists.
00:17:56 Disorders of Platelets: Discusses HUS and TTP, including their pathophysiology, clinical manifestations, and management. Also covers drug-induced thrombocytopenia and inherited platelet function disorders.
🔑 Disorders of Platelets are characterized by endothelial and leukocyte activation with platelet activation involved.
📜 Hemolytic Uremic Syndrome (HUS) is preceded by bloody diarrhea, while atypical HUS is chronic uncontrolled complement activation.
🔬 Thrombotic Thrombocytopenic Purpura (TTP) is characterized by metalloprotease deficiency, resulting in large von Willebrand multimers and micro thrombi.
00:23:56 Disorders of Platelets result from a lack of certain proteins, leading to bleeding problems. Different tests are used for diagnosis, such as platelet aggregation testing. Treatment is usually supportive and may involve platelet transfusions.
Platelets are critical for blood clotting and play a crucial role in activating and aggregating.
Deficiencies in GP one B and the to be 3a can lead to platelet activation and aggregation problems, resulting in bleeding disorders.
Platelet aggregation testing is the gold standard for diagnosing platelet disorders, but it has limitations and may require further investigation.
00:29:56 This video discusses disorders of platelets, including problems with storage granules and inherited disorders of platelet number. Treatment options and potential complications are also mentioned.
📝 Platelet disorders can be caused by the production of antibodies or problems with storage granules.
🔬 Differentiating between alpha and dense granules is important for diagnosing platelet disorders.
💉 Treatment options for platelet disorders include platelet transfusions and stem cell transplant.
🧬 Inherited platelet disorders can be classified as quantitative or qualitative, with associated symptoms and management.
00:35:55 Platelet disorders can be categorized based on platelet size and associated abnormalities. Acquired disorders can be caused by renal failure or certain drugs. Thrombocytosis can be primary or secondary, with essential thrombocythemia requiring more aggressive treatment.
Disorders of platelets can be managed with platelet transfusions, with the platelet count usually increasing after 12-24 months.
There are genetic conditions associated with thrombocytopenia, such as cardio facial syndrome and jacobsen syndrome.
Acquired disorders of platelet function can be caused by renal failure, certain drugs (like aspirin), and cardiac disease.
You might also like...
Read more on People & Blogs
Aula 2 - Tópicos essenciais de Estatística | Semana da Estatística Aplicada | Prof. Fernanda Maciel
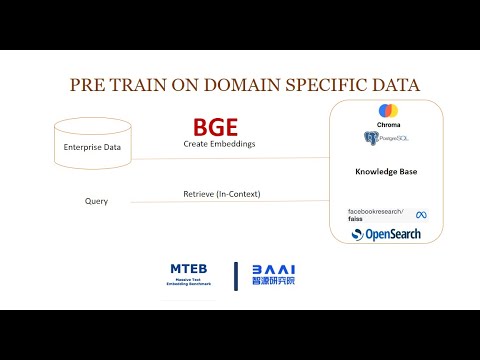
State-of-the-Art BGE embeddings for Retrieval Augmented Generation

La curación mágica de las brujas del susurro | Europa semanal

Hugging Face LLMs with SageMaker + RAG with Pinecone
If I Started a Business Again Today, I'd Do This

Estructura de Datos - Queue - Cola